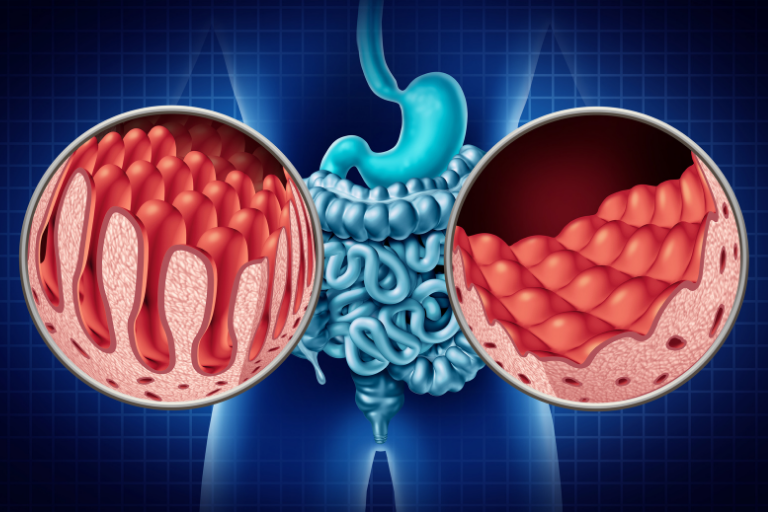
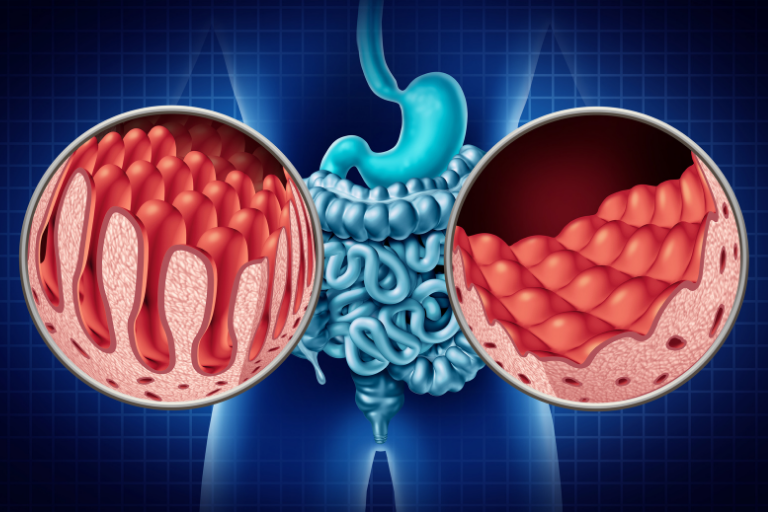
Celiac Disease, also known as gluten intolerance, gluten enteropathy, or non-tropical sprue, is an autoimmune disorder that affects over three million Americans. People with celiac disease cannot digest gluten without triggering a harmful immune response in the small intestine. This can cause intestinal damage which may compound over time.
Heredity plays an important role in the development of celiac disease, with research having identified two genes that are strongly linked to the disorder. Eating gluten is also a necessary part of the development of the disease. There are likely environmental factors that also contribute to gluten intolerance, but what they are specifically is not known.
Digestive symptoms are most common among children. The digestive symptoms identified by the Celiac Disease Foundation include:
- chronic diarrhea
- vomiting
- constipation
- pale or unusually bad-smelling stool
- iron-deficiency anemia
- abdominal bloating and pain
- weight loss
- fatigue
- issues with mood and behavior
- teeth enamel defects
- delayed growth and puberty
- short stature
- Attention Deficit Hyperactivity Disorder (ADHD)
Only one-third of adults with celiac disease have reported digestive symptoms such as diarrhea, but there are a number of other symptoms that may appear. These include:
- iron-deficiency anemia
- fatigue
- bone or joint pain
- arthritis
- osteoporosis (bone loss)
- liver disorders such as fatty liver
- depression
- anxiety
- tingling, numbness, or pain in the extremities)
- seizures or migraines
- missed menstrual periods
- infertility or recurrent miscarriage
- canker sores
- itchy skin rashes
Genetics play a role in the development of gluten intolerance, and you are more likely to be at risk if you have a close relative who has the disorder. Other pre-existing conditions which may increase your risk of Celiac Disease include type 1 diabetes, Down syndrome, autoimmune thyroid disease, microscopic colitis, and Addison’s disease.
Many celiac disease cases are undiagnosed, and it is very possible to have gluten sensitivity without being aware of it. If you are going to be tested for celiac disease, it’s important not to cut gluten from your diet beforehand – a gluten-free diet can cause normal-looking test results even if you have gluten intolerance.
There are two blood tests that may help with detecting celiac disease. Serology testing measures the level of antibodies in your bloodstream, with an elevated antibody protein count suggesting an unusual immune response to gluten. Genetic testing can detect the human leukocyte antigen (HLA) genotype, which appears in 90% of patients with celiac disease.
If the results of a blood test indicate a high likelihood of celiac disease, your doctor may follow up with an endoscopy to take biopsy samples from the small intestine.
 There is currently no known cure for celiac disease, and it can only be managed by sticking to a strict gluten-free diet. This means avoiding foods like wheat, barley, and malt, and also being vigilant of other products which may contain trace amounts of gluten. Avoiding gluten will allow the small intestine to heal over time. Your doctor may also suggest vitamin supplements to make up for any serious deficiencies.
There is currently no known cure for celiac disease, and it can only be managed by sticking to a strict gluten-free diet. This means avoiding foods like wheat, barley, and malt, and also being vigilant of other products which may contain trace amounts of gluten. Avoiding gluten will allow the small intestine to heal over time. Your doctor may also suggest vitamin supplements to make up for any serious deficiencies.
There is no way to prevent celiac disease, but if you have identified one or more of the major risk factors, you should get tested to see if a gluten-free diet may be necessary.
The effects of gluten intolerance are not limited to the digestive system, and can contribute to other harmful conditions including anemia, depression, lactose intolerance, dermatitis herpetiformis (itchy skin rashes), irritable bowel syndrome (IBS), and cancers of the digestive system.
The effects of gluten intolerance are not limited to the digestive system, and can contribute to other harmful conditions including anemia, depression, lactose intolerance, dermatitis herpetiformis (itchy skin rashes), irritable bowel syndrome (IBS), and cancers of the digestive system.
Celiac disease affects roughly one percent of people, and these cases are all-too-frequently undiagnosed. There is no cure for this disease, but a gluten-free diet allows people with gluten intolerance to manage their symptoms and still have a very high quality of life. Digestive symptoms mostly appear in children, but it is also important for adults to get tested if any members of their family have celiac disease, or if they notice ongoing symptoms such as skin rashes, fatigue, depression, or irritability.
 There is currently no known cure for celiac disease, and it can only be managed by sticking to a strict gluten-free diet. This means avoiding foods like wheat, barley, and malt, and also being vigilant of other products which may contain trace amounts of gluten. Avoiding gluten will allow the small intestine to heal over time. Your doctor may also suggest vitamin supplements to make up for any serious deficiencies.
There is currently no known cure for celiac disease, and it can only be managed by sticking to a strict gluten-free diet. This means avoiding foods like wheat, barley, and malt, and also being vigilant of other products which may contain trace amounts of gluten. Avoiding gluten will allow the small intestine to heal over time. Your doctor may also suggest vitamin supplements to make up for any serious deficiencies.
